LGBT-Friendly Provider Spotlight: Dr. Rixt Luikenaar
Guest blog by Tobie Spears
Rixt A. Luikenaar, M.D., FACOG board certified in obstetrics and gynecology, has been providing exceptional healthcare both locally and abroad for over 15 years. She holds numerous awards and continues to receive significant recognition for her work with people of color and the LGBT+ community. Dr. Luikenaar began offering transgender healthcare including hormone therapies, primary care, and preventative care in 2011, which she is continuing to provide at her clinic, Rebirth OBGYN. Dr. Luikenaar works tirelessly to make sure that all people receive the respect and care they deserve. I personally learned much from her and hope you enjoy our interview!
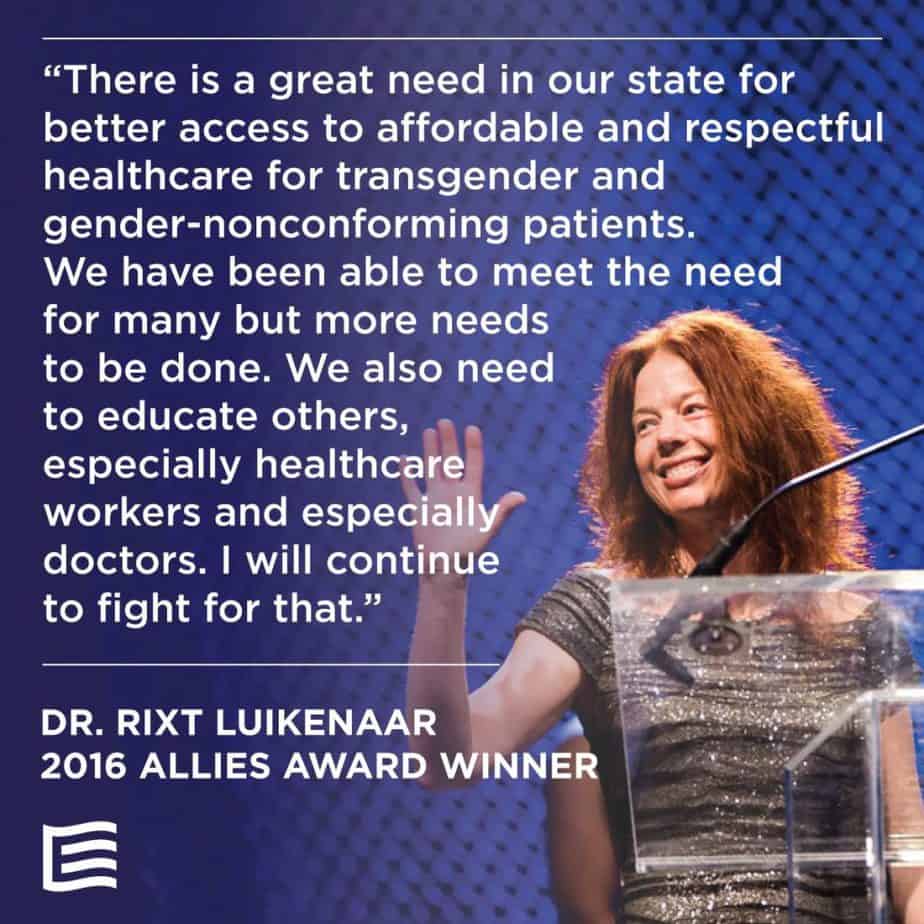
2016 Equality Utah Allies Award Winner
Helpful Terms
Before we get started with the interview, here is a list of terms that may be helpful as you read this post. These were taken from the PFLAG National Glossary of Terms:
Transgender: A term describing a person’s gender identity that does not match their assigned sex at birth. This word is also used as a broad umbrella term to describe those who transcend conventional expectations of gender identity or expression.
Cisgender: A term used to describe an individual whose gender identity aligns with the one typically associated with the sex assigned to them at birth.
Transition: A term used to describe the process—social, legal, or medical—one goes through to discover and/or affirm one’s gender identity. This may, but does not always, include taking hormones; having surgeries; and changing names, pronouns, identification documents, and more. Transgender people may or may not decide to alter their bodies hormonally and/or surgically to match their gender identity.
Non-Binary: A term used to describe those who view their gender identity as one of many possible genders beyond strictly female or male.
LGBT or LGBT+: An acronym that collectively refers to individuals who are lesbian, gay, bisexual, or transgender. May also include the letters Q (for Queer or Questioning) I (for Intersex individuals), P (for polyamorous/polygamist) and A (for Allies).
Gender Reassignment Surgery: Medical interventions used as part of the transition process to affirm one’s gender identity. Also sometimes called gender-affirming surgery, or sex reassignment surgery (SRS).
Interview with Dr. Luikenaar
What led you to be interested in working with transgender individuals?
I am from the Netherlands, and in my last year of residency in OBGYN (in the US) I spent a month in the Netherlands with a doctor/sex therapist that treated transgender patients and they intrigued me. During my time in practice at the University of Utah I realized there was nobody caring for these patients and I felt like taking on the LGBTQ community just as I take on any minority (refugees, Latinos, Native American patients, etc). Interestingly, after I opened my clinic my youngest child, born female, said from the age of 2 that he is a boy. At age 5, all girl clothes were thrown out, and he wanted to be “Alex” and “him” from age 7 on. So we have socially transitioned him into a boy. He is now 10 years old (no pressure there, he knows he can be Sophia anytime he would want to).
During my time in practice at the University of Utah I realized there was nobody caring for these patients and I felt like taking on the LGBTQ community just as I take on any minority (refugees, Latinos, Native American patients, etc).
What services do you provide?
My training is in obstetrics and gynecology; I provide any service related to obstetrics and gynecology but I have had a lot of training in primary and preventive care, and offer transgender hormone therapy and postoperative care after gender reassignment surgery. I perform gynecological surgery from ablations, tubal ligations, to laparoscopic-robotic hysterectomies.
What specialized training have you had?
I did my residency in Obstetrics and Gynecology, and am board-certified. I am self-trained in transgender health, however the World Professional Association for Transgender Health (WPATH) has started a certification program for providers and physicians. I also spent two weeks with the Gender Team at the Vrije Universiteit in Amsterdam (a transgender center that has worked with transgender children and adolescents since the 1980’s). They provide a multidisciplinary approach to transgender health care and are very well known for this.
How is working with transgender people the same or different from working with cisgender people?
If you are used to treating all people equally it is not that hard. Just remember you treat the anatomy that is present and ask for their preferred name and pronouns. Especially in the beginning of transition or if they are non-binary it is better to ask than to presume.

Dr. Luikenaar with transgender actress and activist Laverne Cox
What are some of the unique needs of transgender people?
No unique needs, they just want to be respected. There is a 70% depression/anxiety rate among transgender people, and they are still discriminated overall. They often don’t have insurance or have poor insurance, are often fired from their jobs, and some teens/adolescents are still kicked out of their homes or disowned by their parents. Again, treat the anatomy that is present in primary and preventive care, follow WPATH/Endocrine Society guidelines and discuss fertility/sexuality/contraception depending on their sexual preference. Also, most providers/physicians see gender as a binary; (i.e., you are a man or a woman) and many LGBTQ people don’t think of it this way. Instead, gender is thought of as an “infinity,” a “spectrum” and there is no end and no beginning. Many find themselves somewhere on the spectrum but do not necessarily identify as a transgender man or transgender woman. It is always best not to assume anything, and ask for clarification on people’s preferred pronouns.
Most providers/physicians see gender as a binary; (i.e., you are a man or a woman) and many LGBTQ people don’t think of it this way. Instead, gender is thought of as an “Infinity,” a “Spectrum” and there is no end and no beginning. Many find themselves somewhere on the spectrum but do not necessarily identify as a transgender man or transgender woman. It is always best not to assume anything, and ask for clarification on people’s preferred pronouns.
What should other OBs or midwives be aware of if they get a transgender client so they can provide the best possible care?
I held a “grand rounds” talk for the Department of OBGYN at the U of U and the most important things that I shared were about the Affordable Care Act, and the AMA/ACOG Ethics and Committee Opinions that now say we cannot discriminate who we see. We have to treat these patients and learn about them. I think that learning about transgender health should be a continuing education requirement for healthcare professionals. We already treat many cisgender women with hormones. It is not that hard to extend this knowledge to transgender patients. Also, the ABOG (American Board of OBGYN) stated in 2014 that OBGYNs can now treat men in our clinics. Respect your transgender patients’ names/pronouns, and don’t make assumptions about who they have relationships with. Don’t assume anything, just ask. Don’t ask transgender patients about their genitalia if it is not relevant to the care you are providing. They get tired of explaining why they haven’t had “THE” surgery yet or whether they will ever want to. Some transgender men may want to preserve their fertility to have eggs frozen/transferred to a partner or may want to be pregnant themselves. There are also protocols for transwomen to breastfeed their babies. Uterine transplants so far have not been implanted in transgender women, but I know it is a matter of time; it will be done within the next 10 years. For most doctors, I simply advise to keep your judgements and presumptions at home, come to work to learn and ask questions. That’s what I advise students and residents and they love it.
For most doctors, I simply advise to keep your judgements and presumptions at home, come to work to learn and ask questions. That’s what I advise students and residents and they love it.
In your opinion, what are some of the ongoing unmet needs of the transgender community within healthcare, and how can we as doulas work to meet those needs?
Respect, insurance coverage (two major barriers in healthcare), frank and honest communication, and don’t presume every patient is heterosexual and cisgender.
If you could tell other birth workers one thing to help them best serve the transgender community, what would it be?
Be open minded, tolerant and involve partners and friends in the medical decision-making process. Many transgender people have created “alternative” families, which are made up of friends and other support people, not necessarily their biological family.
Thank you to Dr. Luikenaar for this interview. We appreciate you sharing your knowledge and expertise with the doula community so that we may better serve the LGBT+ community in Utah!


