National Cancer Prevention Month
By: Stacie Rupp, CD(DONA)
laboryourway.com
Stacie has been a birth doula since early 2015 and has recently begun teaching Childbirth Preparation classes through University of Utah Perinatal Education. She loves sharing her excitement about all things birth with expectant couples. She also strives to offer understanding and support to women who have had cancer or who are BRCA+ as they navigate their way along a difficult and life changing path.

When we think of PREVENTING cancer, here are some things that might come to mind:
- Eat healthy
- Don’t use tobacco
- Attain and maintain a healthy weight
- Protect yourself from the sun
- Get regular medical care
- Exercise regularly
- Don’t drink excessively
- Avoid unnecessary exposure to radiation
- Avoid exposure to industrial and environmental toxins
While this is a great list and contains healthy habits we should each follow, I’d like to talk about prevention in a deeper way. I’ll start by sharing my story.
My Story
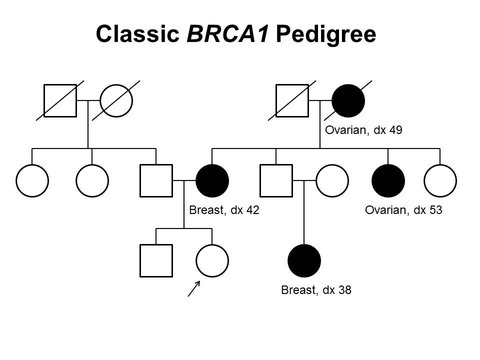
My aunt (my dad’s sister) was diagnosed with breast cancer in her early 40’s (around 2005). While cancer is always scary, hers was caught incredibly early and didn’t seem too devastating. At the time, I was in my early 20’s and just beginning to have children. Because breast cancer at such a young age isn’t incredibly common, my aunt spoke with a genetic counselor. After discussing family health history, other cases of breast and ovarian cancer within our family were uncovered. My aunt decided to have genetic testing done and ultimately tested positive for the BRCA1 gene mutation. You may have heard this referred to as the Breast Cancer Gene. “BR” stands for breast and “CA” stands for cancer.
(Here is a 2 minute video explaining the BRCA gene mutation: https://m.youtube.com/watch?feature=youtu.be&v=UasHCMudOO0)
Huntsman Cancer Institute was conducting a study on the BRCA gene mutations and asked our family to participate. My aunt’s siblings (which included my dad) underwent genetic testing and my dad and another aunt tested positive as well. Many people think/hear that breast and ovarian cancer risk is only passed through females. This is absolutely not the case! My dad’s children and my aunt’s children each had a 50/50 chance of inheriting the gene. I chose to test in 2007 and, while holding my infant son in my arms, was given the news that I was positive. That test result changed so much about the next 10 years of my life.
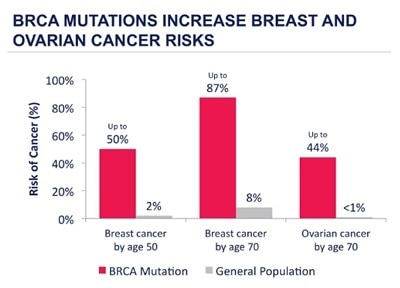
Because of my BRCA1+ status, my genetic counselor and doctors confirmed that my risk for breast cancer was 87% and my risk for ovarian cancer was 65% (varies by individual). Also, the age of cancer onset in BRCA+ individuals is very young. When the odds are so completely stacked against you, and the question is “when” not “if”, the conversation quickly turns to prevention. Ovarian cancer is especially difficult to detect, and once found, is generally in the late stages. Every doctor I spoke with (and I spoke with many) recommended that I prevent by having my breasts removed (double mastectomy) and my ovaries and fallopian tubes removed (salpingo-oophorectomy). Even as I write this now, years later, I feel a wave of nausea come over me.
As doulas, you know the importance of ovaries and breasts. They affect a woman’s identity, fertility, ability to breastfeed, hormones, sexuality, etc. In 2007, at the age of 24, I was not ready to alter my life in such a huge way, by removing these vital organs. So, I chose to do extensive screening instead. I had a mammogram and a breast MRI with contrast annually, alternating every 6 months. I also had a TVUS (transvaginal ultrasound) done each year and a CA-125 blood test, to detect ovarian cancer. Some of my mammograms came back with irregularities, so I was often called back for further screenings. All of this was incredibly draining, both physically and emotionally, not to mention expensive. In the weeks leading up to each screening, I would stress and worry about what they might find (or about what was there that they may not find). Also, waiting for results is the absolute definition of torture.
Thank heavens I did not struggle with fertility. I was able to have 3 children, and my husband and I completed our family. I feel so overwhelmingly grateful that I was able to create, grow, and breastfeed all 3 of my babies. This gratitude continues to grow with each passing year. After I had my last child, I began researching and making plans for preventative (prophylactic) surgeries. I opted (partly for insurance reasons) to have all my surgeries in the same year, 2016. I basically pushed pause on all areas of my life and focused on my health.
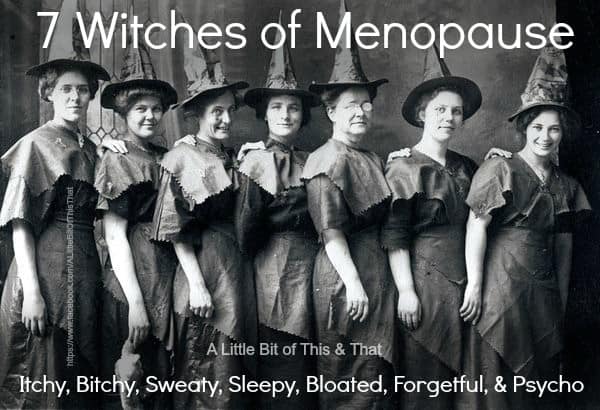
I started with the salpingo-oophorectomy, January 2016, just before my 33rd birthday. Removing your ovaries puts you into instant menopause. I no longer had hormones and so much changed. Some of the side effects included: hot flashes, night sweats, mood swings, weight gain, body odor changes, memory loss, loss of libido, vaginal dryness and pain, fatigue, and dry skin. In the year that followed, I was able to find an amazing endocrinologist who helped me semi-regulate with artificial hormones. This lessened the noticeable side effects, but also will help my bone and heart health long term, which are at risk from early menopause.
In April 2016, I had a nipple sparing double mastectomy. My surgeons cut along the crease under each breast, and removed almost all of my breast tissue, up my chest and out into my armpits as well. I say “almost” all of my breast tissue because removing all breast tissue would require removing the skin as well. They do their best to scrape out the breast cells/tissue, while still leaving enough along the skin to have adequate blood flow. If they scrape too deep, the skin in that area will die and skin grafts will be needed. Breast self-exams and annual doctor visits are still crucial, because caner can still form in the remaining breast cells. I’ve just drastically reduced the odds.
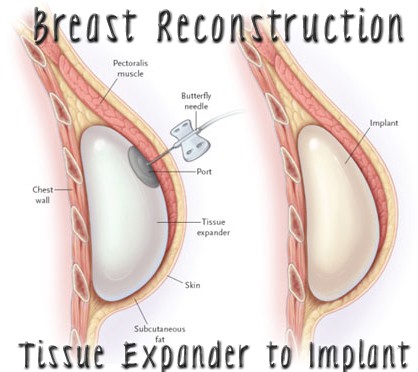
Because I decided on reconstructive surgery, tissue expanders were placed in my empty chest cavities, underneath my chest muscles. These are basically thick plastic balloons that can be filled with saline, through a magnetic port. The chest muscle is normally under a woman’s breast tissue. But, in order to protect my skin and implant, the muscle is lifted and the expander is placed underneath. Over the next months, my surgeon injected saline into my expanders weekly, slowing lifting the muscle. Expanding it all at once would cause excruciating chest pain.
I also awoke from surgery with 4 surgical drain tubes and drainage bulbs. The trauma of the surgery causes excess internal fluid production that can lead to infection if it isn’t removed. For the next few weeks I had to empty and measure the drainage. Actually, my husband and friends were kind enough to help me with this awful job. The range of motion and strength I had in my arms was incredibly limited, so I needed help with most everything. Who knew how connected our chest muscles are to our arms! I was SO glad when the surgical drains were finally removed.

Once I had recovered and my expanders were filled to my old chest size, I had reconstructive surgery, September 2016. The tissue expanders were removed and implants took their place. These will need to be replaced every 10-20 years. Though I now looked “normal” with my clothes on, I certainly did not feel “normal”. I have honestly been amazed at how much losing my breasts has affected me. For starters, my entire chest is now completely numb. Since all of the nerve endings were cut, there is no feeling. The loss of sensation is the thing I miss the most. As wonderful as my surgeons were, things still aren’t perfect and I am a bit lopsided. Surgery might correct this, but I am so tired of surgeries that it isn’t worth it to me. At this point, I’d like give you a high five if you’ve read this far!
I’d also like to address a reaction that some of you might be having. “Why the heck did you have a mastectomy when you didn’t even have breast cancer!?” I can answer this question best with the following analogy. Imagine you are on board an airplane, ready for a journey. The pilot gets on the intercom and says this: “We have run the numbers and thought we’d bring some information to your attention. This particular flight path has been flown thousands of times before, and 87% of the time, the plane crashes. About 9 out of 10 times. Sometimes it crashes in the beginning of the flight. Sometimes in the middle or towards the end. But if you take this journey, you too have an 87% chance of crashing. You may not die in the crash, but really, we just don’t know. There are so many unknown factors. Most other planes, on other flights, only crash 1 out of 10 times. But that’s not the plane you are on. So, think about it. Make the decision that is best for you. There is still time for you to get off the plane, if you choose.” This is how many women with the BRCA gene mutation feel. It’s how I felt, so I chose to get off the damn plane! The decision came after a lot of research and heartache. If you still don’t understand, talk to any woman who has been through breast cancer treatment and see if she wishes she could have avoided it.
Know Your Risk
So what does all of this mean for you??? The science of genetics has made huge strides in recent years. “Know Your Risk” is a catch phrase that encourages people to evaluate their genetic risk for certain types of cancers. Everyone should take the time to talk with family members and write up a family tree of sorts. This can help you uncover cancers that may have a genetic link.
http://www1.cbn.com/healthyliving-17 can help you evaluate if you should speak with a genetic counselor. If you see any red flags, genetic counselors are specially trained to help you assess your risk and can assist you with next steps and possible genetic testing. Be aware that the cost of genetic testing is decreasing every year, with many insurance companies covering costs. So don’t let the possible expense keep you from researching your risk. In terms of breast and ovarian cancers, the website assessyourrisk.org is an incredibly valuable resource. In just a few minutes, you answer questions that help determine your risk. Without knowledge of your risk, you can’t have the power to take preventative steps. Knowledge is power, in a very real sense. While I respect that some BRCA+ women choose to NOT have prophylactic surgeries, I truly believe that the knowledge of my genetic mutation likely saved my life.
Changed For The Better
I obviously would rather be BRCA negative, and I wish I could have avoided these surgeries, but I do feel I am a better person, and doula, because of what I’ve been through. The things I’ve experienced have been life changing, to say the least, and my ability to empathize with others and withhold judgement has increased. I feel better equipped to hold space for those around me, especially my clients. We can’t “fix” what is going on in the lives of others, but we can be present and we can show love. The financial strains of medical bills are familiar to me. Physical pain, endurance, and the bodies amazing ability to heal are thoughts I’d pondered. All of this has also been a reminder that we don’t know why a woman might choose (or have the ability) to have children, to not have children, to have them at a young age, to have them old, to birth one child or to birth a dozen. It is absolutely none of my business. I will love and care for the women who surround me, regardless of their fertility.
I feel particularly equipped to understand women who are having hormone imbalance issues, whether that is during pregnancy, postpartum, menopause, or any other phase of life. I also have gained so much gratitude for the human body, especially the female body. Our reproductive organs are truly miraculous! Let’s embrace and appreciate all they do for us. Breastfeeding is also such a personal experience, and I hope to validate the real mourning process that occurs for women who are unable to breastfeed their babies, for whatever reason. I also want to empower women who desire to breastfeed, but are unable due to mastectomy, to explore their options with SNS (supplemental nursing system) and skin to skin. The bonding and closeness that comes through a mother’s breasts doesn’t need to be tossed aside because milk isn’t produced.
I can relate to the struggles that women have through pregnancy and postpartum as they get used to a new and ever changing body. Body image and identity issues are close to the surface and tug at my emotions. The struggles in an intimate partner relationship are real and difficult to navigate, especially when one person isn’t comfortable in their own skin. But I am here to offer hope. An evolution can take place and comfort with our own body can return, regardless of the destruction that has occurred. A very experienced Labor & Delivery nurse once explained childbirth as being dealt a hand of cards. We don’t get to choose what we’re dealt, but we can equip ourselves to play our hand well. That is the same with each of our lives. We take the cards we’re dealt and we work to play our hand well. I don’t like many of the cards I’ve been dealt, but it turns out, I can still win the game, in my own way.
If you would like to read more details about my story, or to find further information about the BRCA gene mutation, I have blogged about my experience at bonjourkitchen.blogspot.com, January 2016-September 2016. Another wonderful resource is: facingourrisk.org

