Milk Sharing
By: Dezarae Weyburn
After a while, a second nurse came in with a warm bottle for the baby. “Good, the family’s here,” she said. “It’s feeding time.” She handed the bottle to our nurse and then went on to the next baby.
Marie-Thérèse grasped the bottle tightly, and the nurse helped her put it into the baby’s mouth. “What kind of milk is this?” As with most children, Marie-Thérèse’s curiosity knew no bounds.
“Formula,” I said.
“Actually,” the nurse explained, “it’s mother’s milk– most of it a donation from the mothers whose babies are here. They usually express much more than their babies can eat, so they give it to the babies whose mothers are unable to nurse for one reason or another. Mother’s milk is the best thing we can give them; it will help them grow strong faster. Of course, the milk is gathered under very rigid guidelines, so it’s perfectly clean and safe. Because we’ve had so much success with it, our doctors have fought to keep the program in place.”
—Excerpt from Ariana: A Gift Most Precious by Rachel Ann Nunes
My first exposure to breast milk donation came from a book on tape I loved to listen to as a little girl. One of the character’s has a premature infant, and her four year old is brought up with the narrator to meet the baby in the NICU. At the time, I hadn’t given much thought to how babies were fed. I was the youngest, and while my mom babysat, I didn’t pay much attention.
Years later, when I became a mother, my full-term daughter was taken the to NICU as a precaution for a mild fever. I began pumping between feeding her, and by day three, I was making far more than she needed. With Ariana in mind, I asked the nurses if I could donate my milk to the other babies in the NICU, and I was shocked when they said no. I wondered if research had proven that breast milk was not as beneficial as they thought it was back in 1997 when this book was published. I shrugged it off and returned home with my daughter and husband the next day, not realizing that my breasts would continue to overproduce for the duration of our breastfeeding experience.

I once pumped 18 ounces of milk in one go. This is not what a normal supply looks like!
Even when I had my gallbladder out when my daughter was only six weeks old, I didn’t consider checking for donor milk. My experience at the hospital had made me feel as if that wasn’t done, so my daughter was fed from the sample cans of formula I had gotten from my hospital birth class. I was fortunate that breastfeeding resumed after surgery with little issue, but the oversupply hit again with force. I was constantly massaging out clogged ducts, hand expressing in the shower just to release enough milk to allow my baby to latch, and going through dozens of disposable nursing pads per day.
It was exhausting. I purposely started the weaning process when my daughter was eight months old, slowly dropping one feed at a time. At thirteen months old, on January 13, 2014, she nursed for the last time.
Exactly a month later, I found out I was pregnant.
Our second child was not planned, at least, not yet. I had intended to have a bigger age gap. I had intended to have my body to myself for at least a few months. I was dreading breastfeeding again, mentally tallying up the number of nursing pads I would need. I decided to research ways to limit supply. During this pregnancy, I learned about block feeding (link: http://www.nancymohrbacher.com/articles/2013/10/9/block-feeding-dos-donts.html ), and I kept running across stories about milk sharing. I found them interesting, but decided to limit supply anyway.
When my baby was born, I immediately started block feeding. She nursed well and while I still leaked, it was nothing compared to the first year of breastfeeding! I settled into my postpartum period less than gracefully, and spent a lot of time online, trying to escape the dark claws of postpartum depression. During this time, I saw many articles about milk sharing. It felt like something I needed to do, so when she was three months old, I grudgingly began pumping in between feeds, restimulating supply. I grudgingly turned to galactagogues. Milkmaids tea, fennel, and oatmeal became big staples in our home. I pumped more often, and was able to save up about 40 extra ounces. I excitedly joined the local Facebook group for Human Milk 4 Human Babies. I got stuck at “pending approval” for three days that felt like torture! I cannot imagine how much longer it would have felt to have to wait that long to receive milk. I was finally approved, and immediately found a twin family to donate to. We agreed to meet but she was unable to make it.
I tried again with another mom, whose son was only a bit older than my little one. Natalie* lived about an hour and a half away, and I didn’t want her to make that drive for a measly 40 oz. Her son was due for surgery soon, and I knew that breast milk could help him recover. I promised to do whatever I could to get 100 oz or more before I contacted her again. I started pumping four times a day. The dishes were killer, but a cloud was starting to lift. My postpartum depression was easing slightly.
I managed to exceed 100 oz in just a few days, and excitedly texted her to let her know. Her husband drove up to pick it up and replaced the bags I’d used. It was such a rush knowing that I was helping someone.
My supply had definitely increased. My daughter refused to take bottles, so when I started working, I pumped 4-10 oz at work, and it went straight into the freezer for my “milk mamas”. On longer shifts, I sometimes came home with more than 20 oz of frozen milk. Pumping became an escape for me. As long as I got at least 6 oz each time I pumped, I stayed mostly sane and happy. My husband had to remind me a few times to be gentle with myself. Once, while pumping, I lamented that I had only managed to get 4 oz, and he reminded me that some women don’t do that in a full day, let alone in ten minutes.
Perspective was helpful, but the thing that helped most was getting to know one of the families I donated to. Natalie met me at Costa Vida the first time she came up. My girls loved her little boy, and I felt more love and sincere appreciation from her in one afternoon than I had in most of my postpartum experience. (Kids don’t exactly give positive feedback.) She explained some of her feeding problems, the bad advice she was given, and the fact that she was already pregnant again. Her milk supply had been lost quickly, but she was determined to change that with the baby she now carried.
I admired her. Her goal was simple: that her son receive some breast milk every day for a year. Some days that was two ounces, some days it was ten, but she was determined to give him what she could. Once upon a time, I judged women for bottle feeding/formula feeding. Natalie gave me perspective that I absolutely needed, and I no longer do that. It’s none of my business why a baby is fed formula or breast milk. It’s not of my business if a baby is formula fed in the hospital or not. As a human being, my job is empathy. My job is love.
I donated to a few more moms and babies, but I felt that Natalie and her son were ultimately the reason I had felt the pull to donate as acutely as I did. My tally ended up being 8 babies, 7 moms.
I wish that more families realized that a) donor milk is available and b) they can donate excess milk. Even for healthy, term babies, the World Health Organization suggests that breastfeeding should be the first choice when possible, then wet nursing or donor milk, and formula as the last resort. Without normalizing milk sharing, we deprive moms and babies of an option that offers tons of benefits. We also open up an opportunity for women and babies to be exploited, both by formula companies and people that stoop to selling “breast milk” mixed with water or cow milk as a way to make upwards of $4 an ounce. The safest way to milk share is to do it without an exchange of money or goods. Usually the only thing that changes hands is milk, new bags, and on occasion, lactation cookies.
I do plan to donate from the beginning if I decide to have another baby, and the research I’ve done has led me to want to donate both privately and to a milk bank. Private donation is selfishly more about me than it is about the families I’m helping. It is positive feedback and endorphins and friends. It is a way for me to feel like I’m giving charitably when I have so little to give at the end of the day.
Milk banks typically fall into two different categories: for profit and nonprofit. For profit milk banks are often owned by big name formula companies, and they compensate their donors. The milk is not given directly to babies, but is researched or made into “breast milk fortifier”. This is one of the ways that formula companies try to improve their product, and is a good reason to donate. My caveat is to be aware that for-profit milk banks occasionally have a minimum donation quota, which can be stressful.

Image Credit: www.hmbana.org
Non-profit milk banks can be found through the Human Milk Banking Association of America: https://www.hmbana.org/. The nearest milk bank to Utah is in Colorado, but there are donation spots throughout Utah. Arrivals Birth Center in South Ogden has a donation center. The milk donated to these milk banks is homogenized (much the same as cow milk) and sold to NICUs for the lowest possible cost, although it still ends up costing $3-$5 an ounce. Because human milk is so good at eliminating risk of NEC (http://pediatrics.aappublications.org/content/early/2016/02/19/peds.2015-3123), it is usually rationed to the smallest or sickest babies. More donors could mean more lives saved. You can find more information about local Utah milk donation by visiting the Mountain West Mother’s Milk Bank website: https://www.mwmothersmilkbank.org/.
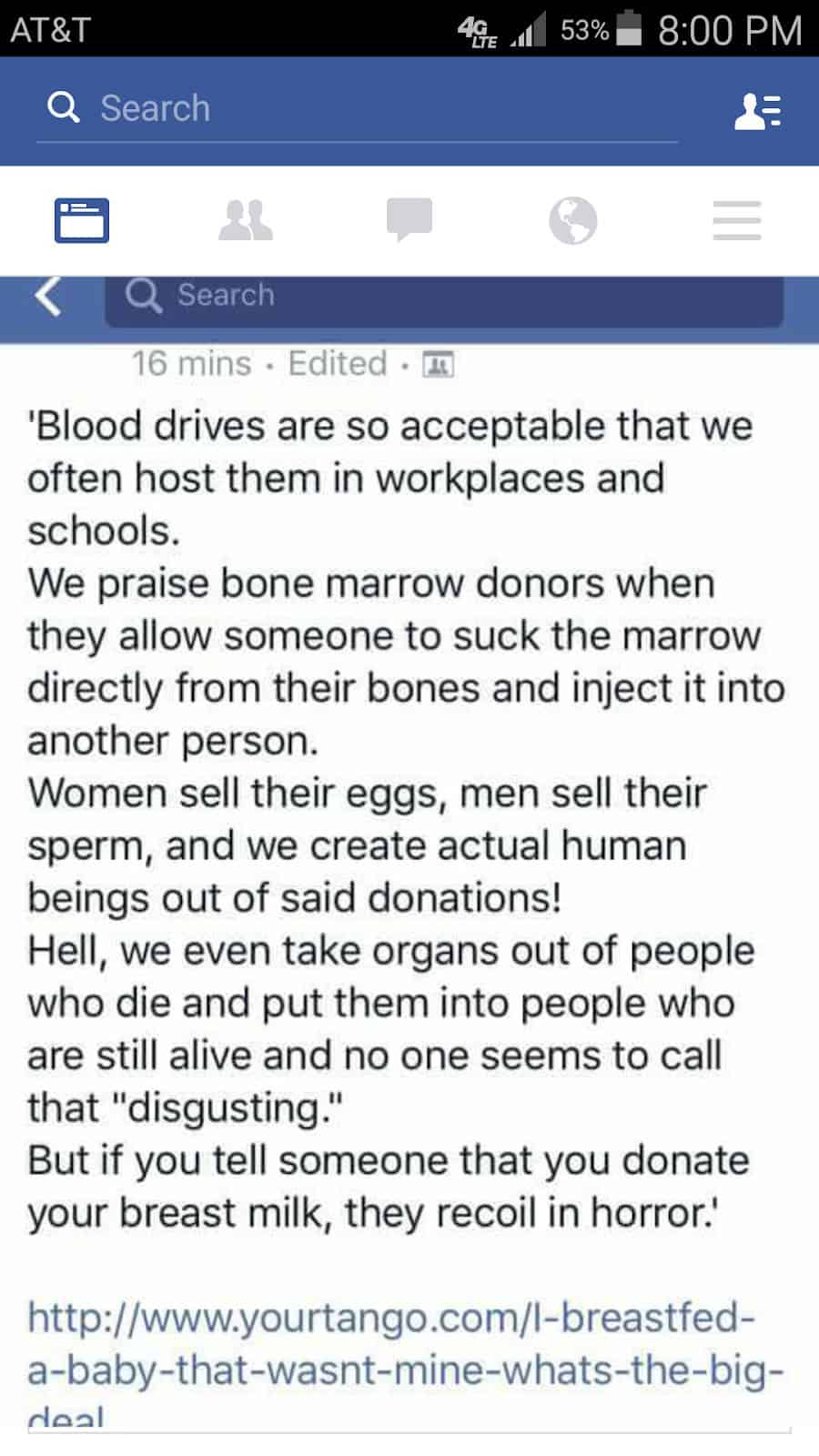
I urge everyone to open up dialogue about donor milk. Make it normal. We host blood drives in public spaces and nobody cares, but I mention that I’m a milk donor and people raise their eyebrows. Blood and milk can both save lives. I can’t wait until it is normal to share milk. Until women no longer feel like their only option is that can of formula in the cupboard when they have to go to surgery and leave their newborn baby at home. It can start with you.
*Name changed for privacy
About Dezarae:

